What Actually Helped My Postpartum Recovery (It Wasn't What I Expected)
Everyone told me to get outside. Exercise. Ask for help. Sleep train the baby (🙄).
I didn’t know what I needed. I'm an occupational therapist—I understand the importance of movement, sleep, and support systems. But one year into postpartum and I couldn’t bring myself to do any of it.
I was experiencing more hair loss, brain fog, and mood swings than I was comfortable with—the kind that a good night of rest didn't fix. I kept being told these were "normal" postpartum experiences. That it would get better with time.
But something was missing.
It took me over a year to figure out what. And when I did, I realized I'd been overlooking the most fundamental piece: my body was nutritionally depleted.
Once I knew more, I realized the prenatal I was taking wasn't even close to replenishing what I'd lost.
The Depletion No One Talks About
As an OT, I knew nothing about postpartum depletion. It isn’t something we learn about in school. I had to complete extensive continuing education and read about it in research.
Here's what I didn't know then: up to 95% of women experience nutritional depletion, even when taking a prenatal vitamin.
Pregnancy, birth, and breastfeeding make enormous demands on our bodies. We're literally building another human, possibly recovering from birth trauma (whether vaginal or surgical), and producing milk—all while running on minimal sleep.
Our bodies need specific nutrients to carry out these functions: vitamin D for immune health and mood regulation, choline for baby's brain development and our own cognitive function, B vitamins for energy metabolism, iron and zinc for hormone production.
When we don't get enough of these nutrients, depletion manifests as occasional fatigue, brain fog, hair loss, mood changes—all the symptoms I was experiencing. All the symptoms I'd been told were "just part of postpartum."
But here's the kicker: National health data (NHANES) shows that even women who take supplements are often still deficient in key nutrients, including vitamins D, A, B6, choline, magnesium, iron, and zinc.
These aren't "nice-to-haves." They're critical for healthy hormone production, cognitive function, energy, and yes—mood regulation.
Why Most Prenatals Fall Short
When I started looking at my own prenatal vitamin, I realized it was based on something called RDAs—Recommended Dietary Allowances.
These sound official. Science-based. Trustworthy.
But here's the problem: Pregnant and breastfeeding women were excluded from 83% of the studies that informed these standards.
Seriously?! 83%.
The nutrition guidelines we're told to follow during pregnancy and postpartum were created using research on men and non-pregnant women.
RDAs were designed in 1941 to define the minimum amounts needed to prevent deficiency, not the optimal levels for health. And they definitely weren't designed for the increased demands of growing a baby, recovering from birth, or producing milk.
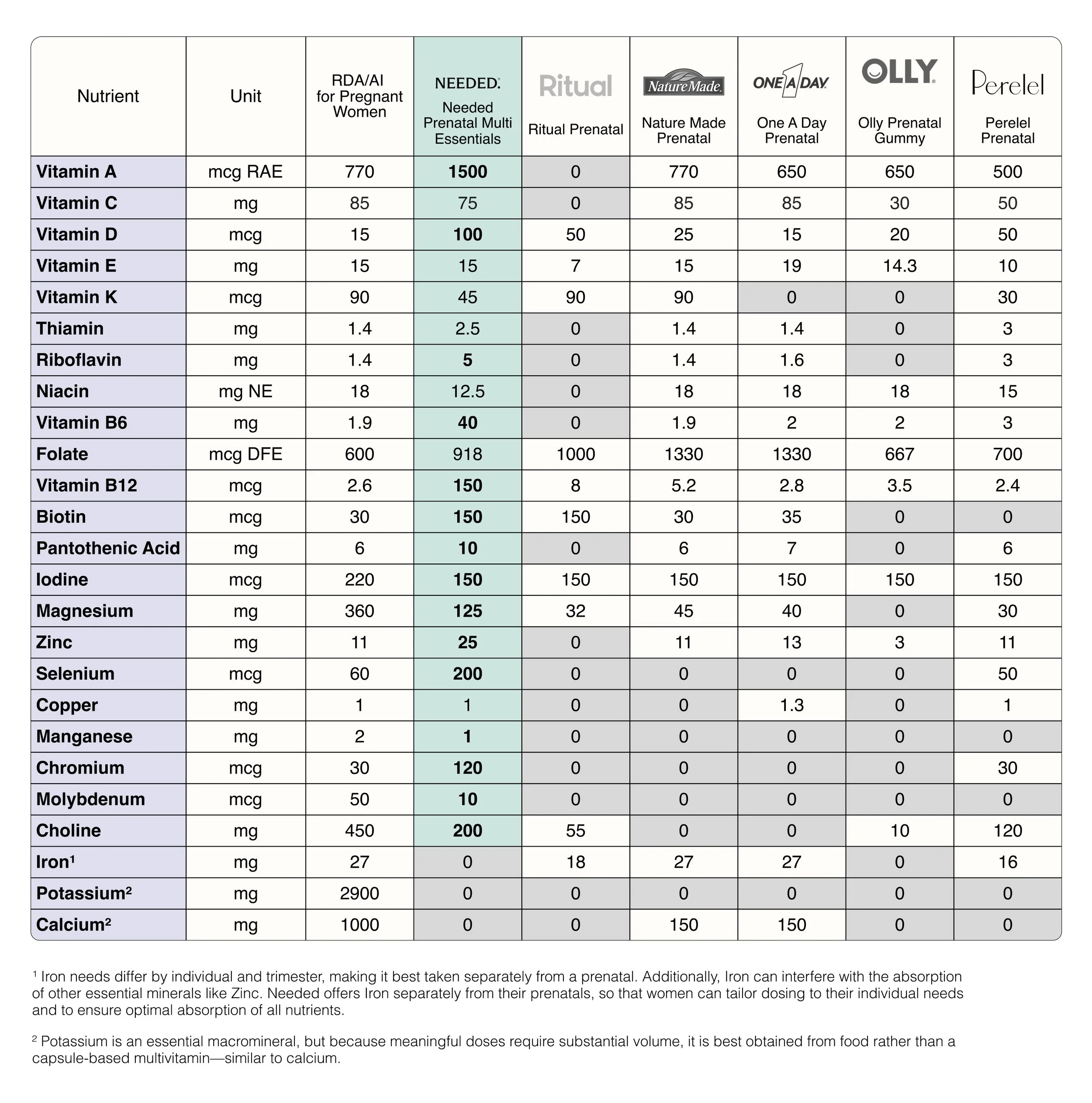
As a result, most prenatal vitamins provide bare minimums using less-than-ideal forms of nutrients. They're formulated for adequacy, not repletion. And some of the leading prenatals, dose even below outdated Recommended Dietary Allowances for most nutrients.*
And when you're already depleted? Adequacy ain't enough.
Needed Prenatal Multi provides 8x more nutrition than leading prenatals.*
What Changed for Me
I started looking for a prenatal that was actually formulated for the demands of pregnancy and postpartum. Not just meeting outdated minimums, but addressing real nutritional needs.
That's when I found Needed Prenatal Multi.
It provides methylated folate (not synthetic folic acid), active nutrient forms for better absorption, and clinically studied dosages of vitamin D3, choline, and other nutrients that support health throughout pregnancy and postpartum.
Soon enough, I noticed a shift after switching. Mostly in the brain fog lifting. This gave me enough clarity and capacity to do the thing I needed most– curate my support system. My hair loss slowing down was a bonus.
It wasn't magic. It was my body finally getting what it needed to replenish itself.
The Rest of the Puzzle
I need to be clear: nutrition wasn't the only answer.
I still needed to find a breastfeeding-friendly therapist. I still needed sleep support (I eventually trained in CBT-I for insomnia because of this). I still needed community—other parents who actually understood what I was going through. I still needed to move my body, even when it felt impossible.
But nutrition was the foundation I'd been missing.
Once my body had what it needed—the building blocks for hormone production, neurotransmitter synthesis, energy metabolism—everything else became possible.
I could show up for therapy and string together thoughts. I could connect with my baby without the constant dread. I could start finding my way to a new version of me.
The depletion had been real. The symptoms weren't "just postpartum" or "just in my head." My body was literally struggling to function without the nutrients it desperately needed.
And the prenatal I'd been taking—the generic one I'd grabbed off the shelf at the pharmacy because it was affordable and the OB said it didn’t matter—wasn't designed to address that level of need.
If You're Struggling Too
If you're in the thick of postpartum right now and something feels off—even if you're taking a prenatal—it's worth looking deeper.
Your body might be depleted in ways you don't realize. The symptoms you're experiencing might not be "just part” of postpartum.
You deserve nutrition that actually meets your needs. Not minimums based on outdated research. Not bare-minimum dosages that leave you deficient even while supplementing.
I suggest my clients look into Needed Prenatal Multi because it's what I wish I'd had from the beginning.
And if you're still struggling with mood, energy, or cognitive function postpartum—even with better nutrition—please reach out for support. To a therapist, to your primary provider, to someone who can help you figure out the root cause of what else might be going on.
Your struggle is real. And you deserve care that actually addresses what you're going through—not dismissal disguised as reassurance.
References
Bailey, R. L., Pac, S. G., Fulgoni, V. L., 3rd, Reidy, K. C., & Catalano, P. M. (2019). Estimation of Total Usual Dietary Intakes of Pregnant Women in the United States. JAMA network open, 2(6), e195967. https://doi.org/10.1001/jamanetworkopen.2019.5967
Emily R. Smith et al.,Limited data exist to inform our basic understanding of micronutrient requirements in pregnancy.Sci. Adv.7,eabj8016(2021).DOI:10.1126/sciadv.abj8016
This post is sponsored by Needed, a brand I genuinely educate my clients about and use personally.
These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
**Based on Recommended Dietary Allowances, compared to leading prenatals as determined by IRI sales data as of December, 2025.
*Based on the total daily dosage of nutrients provided compared to leading prenatals as determined by IRI sales data as of December, 2025.